New Zealand Health Data Landscape (Online)
Advance your understanding of how routinely collected data can support health care decision-making. Apply NowTalk to an AdvisorNew Zealand Health Data Landscape (Online)
Advance your understanding of how routinely collected data can support health care decision-making. Apply NowTalk to an AdvisorMEDICAL & HEALTH SCIENCES
New Zealand Health Data Landscape (Online)
Certificate of Proficiency | Contributes to PGDipHSc in Digital Health
Advance your understanding of how routinely collected data can support health care decision-making with this 15-point credit bearing course comprising 12 weekly modules.
Recommended Background
Students will have a relevant degree or health qualification
University Entrance (or equivalent required for admission)
Duration
12 weeks
Next Start Dates
21 July 2025 (Semester Two)
Applications close one week before the course starts. Apply early to secure your spot.
Domestic Fees
$1,361.55 (estimate)
Disclaimer: *Fees are inclusive of 15% GST, but do not include the Student Services Fee, course books, travel and health insurance, or living costs. Amounts shown are indicative only. In addition to the tuition fee, there is a Student Services Fee of $4.44 per point (online). Fees will be confirmed upon completion of enrolment into courses.
Why is this course right for you?
This course is part of the Postgraduate Diploma in Health Sciences (PGDipHSc) in Digital Health and may also be taken as a course-only study option. It provides an overview of key issues to support the appropriate and effective use of large volumes of routinely collected data to drive improvements in the delivery of health care. Ethical and equitable use of health data, critical evaluation of health data, identification of analytic methods and appropriate interpretation to support health care decision-making are discussed. Specific datasets are not analysed.
Upon completion, students who wish to progress their studies further towards a formal qualification may count this course towards the PGDipHSc in Digital Health (entry criteria and time limits apply).
Clinicians, health service managers and analysts, along with researchers, are able to access an increasing array of routinely collected repositories of “big data” from health and other sectors that can be linked using New Zealand’s unique national identifier – the National Health Index number. This health data landscape provides tremendous opportunities for improving the delivery of population and personalised health care and providing efficient mechanisms for undertaking research on a large scale. Along with this potential though are significant pitfalls that need to be considered in order to optimise the use of such data and avoid its misuse.
In this course you will explore the ethical and equitable use of health data, critical evaluation of the quality of data and information available in New Zealand, and the framing of questions and interpretation of findings using available data and information to support robust health care decision-making.
Course |
Description |
||
| Sources and limitations of routinely collected data and analyses for the New Zealand health sector | This week introduces students to descriptions of data, big data and routinely collected electronic health data. The challenges in turning big data into actionable clinical and health intelligence are illustrated. Major sources of routinely collected electronic health data in New Zealand are described, as well as major sources of analyses of routinely collected health data. An introduction to the Integrated Data Infrastructure (IDI) and data linkage is provided. | ||
| Data life cycle and quality issues | This week’s module covers the key steps of the data life cycle and key factors that may affect the quality of routinely collected electronic health data, including examples. | ||
| Population health perspective and burden of disease | This week’s module provides a definition of population health (in comparison to personal and public health) and the implications of this for health information systems. We cover what is meant by “burden of disease” and how this can be assessed as part of a health needs assessment, which is a part of the DHB planning cycle. | ||
| Equity | This week’s module focuses on health equity and big data using the example of cardiovascular disease | ||
| Study quality and reporting | This week introduces students to frameworks that are available to assess the quality of study conduct and reporting for different study types, including the EQUATOR network and RECORD statement. | ||
| Risk of bias | This week’s module provides an overview of tools that are available to assess risk of bias for different study types, with a particular focus on the Cochrane Tool to Assess Risk of Bias in Cohort Studies. | ||
| Ethics and social licence | This week’s module considers the ethical and social license issues that emerge in relation to secondary use of data. | ||
| NZ health data strategy and data sovereignty | This week’s module considers key aspects underpinning the national data information strategy for the health and disability sectors and provides an overview of Māori data, Māori data sovereignty and Te Mana Raraunga. | ||
| Optimising current data and collecting new data | Using case studies, this week’s module explores: – the key principles to consider for database design and structure for new data – challenges in creating and maintaining efficient methods of new data collection – methods that can be used to optimise the use of current data |
||
| Indicators | This week’s module defines health indicators, explains their use and limitations in their use, and how they can be monitored over time using run and control charts. | ||
| Dashboards and other visual representations of data | Using examples from Waitematā DHB, this week’s module illustrates the visual representation of data including dashboards as a data visualisation/navigation tool. | ||
| Analytic methods | This week’s module provides an overview of analytical methods (descriptive, predictive, causative) and when each method might be appropriate to use. |
Programme Structure
In this course you will develop knowledge of the biological processes underpinning neurological recovery after stroke. You will also develop interdisciplinary understanding of assessment and interprofessional treatment strategies for impairments in communication, swallowing, vision, sensation, cognition, continence, and movement. Skills in assessing independence and participation using standard scales will be also be developed for application in clinical practice.
Sources and limitations of routinely collected data and analyses for the New Zealand health sector
This week introduces students to descriptions of data, big data and routinely collected electronic health data. The challenges in turning big data into actionable clinical and health intelligence are illustrated. Major sources of routinely collected electronic health data in New Zealand are described, as well as major sources of analyses of routinely collected health data. An introduction to the Integrated Data Infrastructure (IDI) and data linkage is provided.
Data life cycle and quality issues
This week’s module covers the key steps of the data life cycle and key factors that may affect the quality of routinely collected electronic health data, including examples.
Population health perspective and burden of disease
This week’s module provides a definition of population health (in comparison to personal and public health) and the implications of this for health information systems. We cover what is meant by “burden of disease” and how this can be assessed as part of a health needs assessment, which is a part of the DHB planning cycle.
Equity
This week’s module focuses on health equity and big data using the example of cardiovascular disease.
Study quality and reporting
This week introduces students to frameworks that are available to assess the quality of study conduct and reporting for different study types, including the EQUATOR network and RECORD statement.
Risk of bias
This week’s module provides an overview of tools that are available to assess risk of bias for different study types, with a particular focus on the Cochrane Tool to Assess Risk of Bias in Cohort Studies.
Ethics and social licence
This week’s module considers the ethical and social license issues that emerge in relation to secondary use of data.
NZ health data strategy and data sovereignty
This week’s module considers key aspects underpinning the national data information strategy for the health and disability sectors and provides an overview of Māori data, Māori data sovereignty and Te Mana Raraunga.
Optimising current data and collecting new data
Using case studies, this week’s module explores:
– the key principles to consider for database design and structure for new data
– challenges in creating and maintaining efficient methods of new data collection
– methods that can be used to optimise the use of current data
Indicators
This week’s module defines health indicators, explains their use and limitations in their use, and how they can be monitored over time using run and control charts.
Dashboards and other visual representations of data
Using examples from Waitematā DHB, this week’s module illustrates the visual representation of data including dashboards as a data visualisation/navigation tool.
Analytic methods
This week’s module provides an overview of analytical methods (descriptive, predictive, causative) and when each method might be appropriate to use.
Course Benefits
Students who complete this course will be able to:
- Critically evaluate strengths and limitations in the quality of routinely collected New Zealand health data to optimise the integrity of decision-making based on these data
- Interrogate potential benefits and harms from routinely collected data outputs in relation to population health and inequities
Upon successful completion of the course you will:
- Be awarded with 15 credit points from the University of Auckland
- Have the option to take your credit into the PGDipHSc in Digital Health (entry criteria and time limits apply)
Frequently asked questions about this course
Application FAQs
What are the entry requirements?
This course is for students with a relevant degree or health qualification. Relevant subjects include health sciences, nursing, medicine & surgery, pharmacy, optometry, physiotherapy, dental surgery, medical laboratory science, and clinical psychology. Please note that for admission you must meet the requirements to study at a New Zealand University (e.g. through University Entrance or an alternative entrance pathway).
What is the date for the next intake?
The next start date for this course is 15 July 2024 (2024 Semester Two). Enrolment closes one week before the course starts. Enrol early to secure your spot.
Is the course fee a one-off lump sum?
Yes, the course fee is a one-off sum of $1,277.25 for domestic students.
Is this course open to non-resident students?
No. Currently Auckland Online Certificates of Proficiency are only open to NZ citizens and permanent residents.
Studying FAQs
Can I study the course in my own time? Is it suitable for those working full-time?
Yes. You can study at a time that suits you (within the allocated course dates). Auckland Online courses are designed for working professionals. They are flexible yet structured to help you gain the knowledge in the time you have.
How is the course structured?
The course will run over 12 weeks (with a break in the middle), and will comprise 12 weekly modules. Further details on the course structure can be found under the ‘Course Structure’ tab further up on this page.
Assessment FAQs
How will I be assessed?
Learners will be assessed through four assignments that address the learning objectives from each of the modules in the course.
Benefits FAQs
What is a Certificate of Proficiency (CoP)?
A Certificate of Proficiency (CoP) is a course-only study option that allows you to take a course at the University of Auckland, without studying a full programme. It is a good option for those who want to study short-term or to test whether a subject is something they wish to pursue more of in the future.
Does the course enable me to take further study at the University?
If you decide to progress your studies further towards a full qualification, you can apply to reassign the points from your CoP to the PGDipHSc in Digital Health (entry criteria and time limits apply).
How many course credits will I attain upon completion of the course?
Upon completion of the course, you will be awarded with 15 credit points from the University of Auckland.
Do I get a certificate at the end?
As a Certificate of Proficiency is not a formal qualification, you will not be able to graduate with it or receive a graduation certificate. Your results will be recorded on your official academic transcript, providing evidence of your study.
Start Your University Application
Before we transfer you to the University of Auckland application portal to start your application, we would like to capture a few details.
These details enable us to provide you with ongoing information about this course, including exciting updates or any upcoming webinars. Our advisors may also contact you to see if you require any personalised advice to guide you through the application process.
Experimenting with programming in the browser
How to Learn the Basics of Programming? Getting started with programming can be a daunting prospect. Reading code can seem like you're reading a foreign language. Also, there are a huge amount of resources available online - but where do you start? Today we'll be...
Educational Leadership During Challenging Times
The pandemic has pushed us to make change, to transform our practice, to relate to each other in new ways and to think differently about what it means to learn and lead and how learning and leadership happens. As leaders under these conditions we can sometimes...
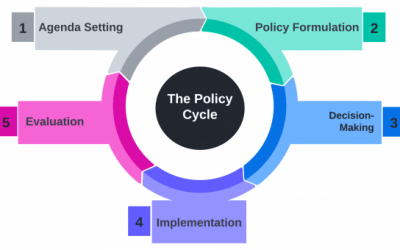
Perspectives in Public Policy – The Policy Cycle
What is Public Policy? According to Wilson (2009), public policy is what governments decide to do, or not do, and their explanations for the outcomes of those decisions in the real world. A recent example of this is the government's 2019 cash injection into the mental...